Harlekin ichthyosis (Harliquin)
This is the most severe
keratinization disorder. The children are encased at birth by a thick
keratotic armor. Thick yellowish plates are present which may crack
forming deep fissures. Movements of the arms and legs is impaired. Those
children who have an extreme manifestation often die within the first
weeks despite intensive care. However, there are also many cases who
take a much milder course and from a clinical perspective there are
cases of transition between very severe collodion baby and Harlekin
ichthyosis. In such cases the drug acitretin - in Germany the brand name
is Neotigason® - can be extremely helpful as it is possible to achieve
within short time the detachment of the much thickened horny layer. In
later life those cases surviving the critical period as a neonate the
skin condition corresponds to that of very severe and at the same time
very inflammatory (erythrodermic) types of lamellar ichthyosis. In this
type the scales remain large. Later the children have difficulties to
gain weight and look "undernourished".
Bullous congenital ichthyosiform
erythroderma of Brocq
This is an uncommon autosomal
dominant keratinization disorder affecting the entire skin and featuring
at birth erythema scaling and blister formation. At birth one usually
notices a complete reddening of the skin with a detachment of the upper
layers of the skin. This may look rather horrible and more dangerous
than it really is. The detachment of the skin is rather superficial and
usually resolves within a few days. Actually there is a true blister
formation of the skin. However, as the blisters form at a very high
level the roof of the blister is easily lost so that one does not see
always intact blisters. The sensitivity of the skin and the proneness
for blister formation is quite variable. Some affected children have
blisters for a couple of days after birth only while in others the
proneness for blister formation remains for many years. Critical periods
can be in the summer when the weather is hot. With increasing age fewer
blister occur, while instead the keratinization becomes more prominent.
The appearance is different from that in most type of lamellar
ichthyosis as the scales are not "lamellar" or platelike but rather
keratotic spines are present.
At the histological level the blister
formation is caused by a characteristic alteration. Therefore usually a
definite diagnosis can be established by a skin biopsy and histologic
and ultrastructural examination of this specimen. The molecular causes
are known today. The disease is due to mutations in the genes for
keratin1 and keratin10. As discussed above these keratins are needed for
the formation of fibril-like structures/filaments or tonofilaments.
These filaments have an important function for the stability of the
cells. If a wrong keratin is incorporated into such a fibril this fibril
will not function properly and the cells loose stability when a
mechanical friction occurs: the result is a blister. Why the prominent
keratosis/keratinization disorder results is not really clear. However,
one has to keep in mind that the tonofilaments insert into structures
called desmosomes and these desmosomes in the end also form part of the
cornified envelope. In this sense bullous congenital ichthyosiform
erythroderma is also a disease of the cornified envelope.
Comèl-Netherton syndrome
In the US and English literature this
disease is today Netherton syndrome called only although it was first
described under the name of "ichthyosis linearis circumflexa" by an
Italian namely Dr. Comèl. This is a rare autosomal recessive
keratinization disorder featuring congenital ichthyosis, a marked
inflammation of the skin at birth/the red neonate and peculiar hair
anomalies. At birth the skin is usually universally red. Later on the
skin condition may improve markedly and round or gyrate scale formation
can develop and often circinate, annular patches are bordered by
distinctive, double-edged scales. These patches are erythematous and can
move on the skin meaning that they appear in some places in particular
on the trunk and after some time disappear to reappear somewhere else.
When looking at the hair under the microscope typical invaginations can
be found of the hair shaft resembling that of the nodes of a bamboo.
Therefore these invaginations are often called in German bamboo hair,
the medical term would be "trichorrhexis invaginata". At the places of
these invaginations the hair shaft can break easily. A further feature
many doctors are not aware of is that the hair can be pulled out rather
easily it does not adhere to the scalp as firmly as normal hair does.
Quite a few children suffer from more
severe types of the Netherton syndrome featuring at birth a marked
erythema of the skin which remains present in later life. In these
children the type of ichthyosis can be rather difficult to distinguish
from those of other types of autosomal recessive congenital ichthyosis
and even from other inflammatory skin disease such as Ommen syndrome,
seborrhoic dermatitis or atopic dermatitis. Children with the more
severe type of Netherton syndrome frequently have problems with the
immune system in particular a proneness to infections, fever,
malnutricion and growth retardation.
If one consider to treat children
with Netherton syndrome with acitretin at all it should be kept in mind
that the dosage has to be very low because otherwise irritations and a
worsening of the skin condition can result.
The molecular cause of Netherton
syndrome are mutations in the gene SPINK5 which encodes a protein that
is called LEKTI. LEKTI is a protease inhibitor and inhibits enzymes
having a trypsin or chymotrypsin-like activity in the skin.
Figure 1:
Neonate suffering from Netherton syndrome. The entire skin is inflamed
and red ("Erythroderma"). The inflamed skin is very permeable for water
resulting in increased transepidermal water loss. This means that
neonates have a high risk of dehydration in the first weeks of life and
need intensive care in the pediatric unit.

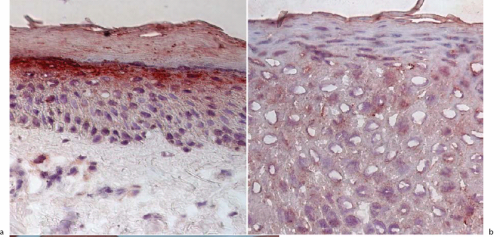
Figure 2:
LEKTI deficiency in a child suffering from Netherton syndrome are a)
positive staining of the skin for LEKTI in normal skin in the stratum
granulosum, b) lack of LEKTI in the skin of a patient with Netherton
syndrome.